(rollover to compare with normal) |
|
Ventricular Septal Defect and the Adult Patient
This common congenital heart defect may occur by itself or in association with other anomalies. Some examples of the latter are Tetralogy of Fallot, Double Inlet Left Ventricle, and Truncus Arteriosus. This discussion is concerned with cases in which one or more ventricular septal defects (VSDs) occur without the presence of other kinds of heart defect.
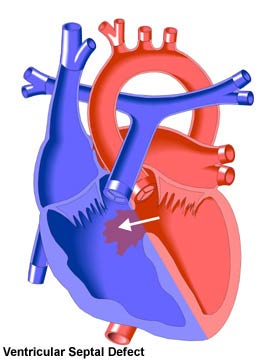
A VSD is a hole in the muscle wall between the two ventricles that allows the movement (shunting) of blood from one ventricle into the other. The direction of shunting will normally be from the left to the right because of the higher pressures in the left heart. In general, the larger the defect, the more shunting of blood will occur.
The left to right shunting of blood through the VSD causes increased blood pressure in the right ventricle and heavy pulmonary blood flow. If untreated, this can cause irreversible changes in the pulmonary circulation as well as a right to left shunt through the VSD and the development of Eisenmenger Complex. The high pulmonary blood flow can also lead to volume overload in the left side of the heart, resulting in enlargement (dilatation) of the left atrium and left ventricle. Over time, this enlargement can lead to congestive heart failure or the occurrence of arrhythmias (irregularities of the heart's rhythm).
Small ventricular septal defects, which did not close spontaneously in childhood, result in a distinctive heart murmur. Larger defects may cause shortness of breath and other problems caused by excessive pulmonary blood flow. Over time, this may lead to pulmonary vascular disease. Accordingly, it is important that larger VSDs are diagnosed and closed surgically as early in life as possible.
The prognosis for patients whose VSDs either closed spontaneously or through surgery before the development of pulmonary vascular disease is excellent, with no exercise restrictions and normal life expectancy. Less than 6% of operated patients will require a follow-up operation to close new or residual VSDs. The later in life a larger VSD is closed, the more likely high pulmonary blood pressure and its attendant complications and lifestyle restrictions will be.
Current forms of VSD repair are usually comparatively low risk procedures. However, some earlier surgical treatments and techniques may lead to complications in later life. These include the development of ventricular dysfunction, aortic regurgitation, arrhythmias, and heart block. Therefore, the operated VSD patient should be checked periodically for the development of symptoms.
Small VSDs that remain open may cause difficulties as a patient ages. Endocarditis (infection of the heart's internal lining) may occur. Arrhythmias (especially atrial fibrillation) may develop, often because of enlargement of the left atrium. The aortic valve may be damaged if the VSD is adjacent to it, resulting in regurgitation and the potential need for valve repair or replacement. There may also be a decrease in exercise tolerance and there is the risk of sudden death. If the symptoms are sufficiently serious, a VSD may be closed late in life. This may be done through open-heart surgery or through a cardiac catheterization procedure, depending on the size of the defect and other factors.
Those patients who received early VSD repair will require medical follow-up. Patients with small open VSDs may be monitored by their local physicians. However, those with moderate to large-sized defects, or with pulmonary vascular disease, are usually advised to undergo regular examination at an adult congenital heart disease center. |